Posture with Clinical Pilates: 4 Exercises to Try at Home
By Chelsey Schwarzenberger, Physiotherapist
As we move into the colder months of the year, we spend more time indoors, which results in us sitting a lot. More sitting means more aches and pains in our neck and shoulders that weren’t there during active summer months. Oh, how we miss being more active and enjoying the hot weather!
For those knots between your shoulder blades and that tightness through your neck and chest, we suggest Clinical Pilates! Clinical Pilates is a form of physiotherapy-based exercise which focuses on muscle control, flexibility, and strength. This treatment is an effective way to increase your postural strength to better cope with sitting and other postural stressors.
Give these four Clinical Pilates exercises for posture a try at-home… you won’t regret it and might find that Clinical Pilates is right for you!
Four Clinical Pilates Exercises to Try
Exercise 1: Spine Twist
The Spine Twist exercise is beneficial for improving the movement in your upper back. Follow these steps for this Clinical Pilates exercise:
- Start by sitting cross-legged, with your head tall and your arms bent and stacked in front of you.
- Draw your abdominal muscles gently inwards towards your spine and take a breath in.
- As you breathe out, keep your hips still and rotate your torso to the left, until you feel a stretch through your middle back.
- Take a breath in and hold this position, then exhale and return to the starting position.
- Repeat this movement again, now moving to the right.
- Complete this sequence 6 times per side.

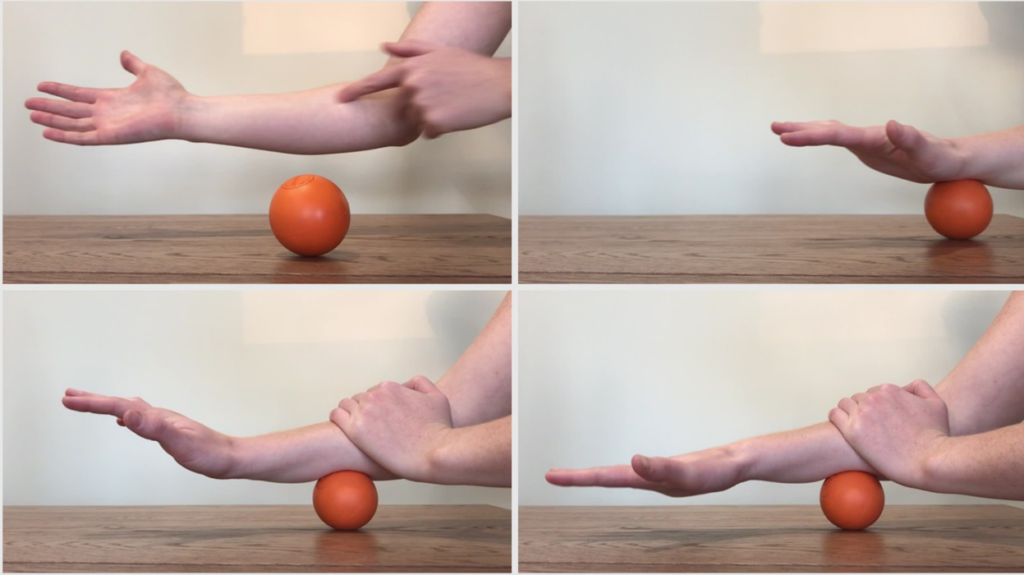
Exercise 2: Breast Stroke Preparation
This Clinical Pilates exercise works on strengthening your neck and shoulder blade muscles.
- Lie on your stomach with your forehead propped up on a rolled towel.
- From here, gently draw in your abdominal muscles and squeeze your shoulder blades down and back like you are trying to pinch a grape between the lower part of your shoulder blades.
- If step two felt easy and you don’t feel your shoulders creeping up towards your ears, you can repeat this but now hover your arms off the mat and gently float your head off the towel, keeping your neck long.
- Hold each repetition for 5 seconds and repeat 10-20 times.


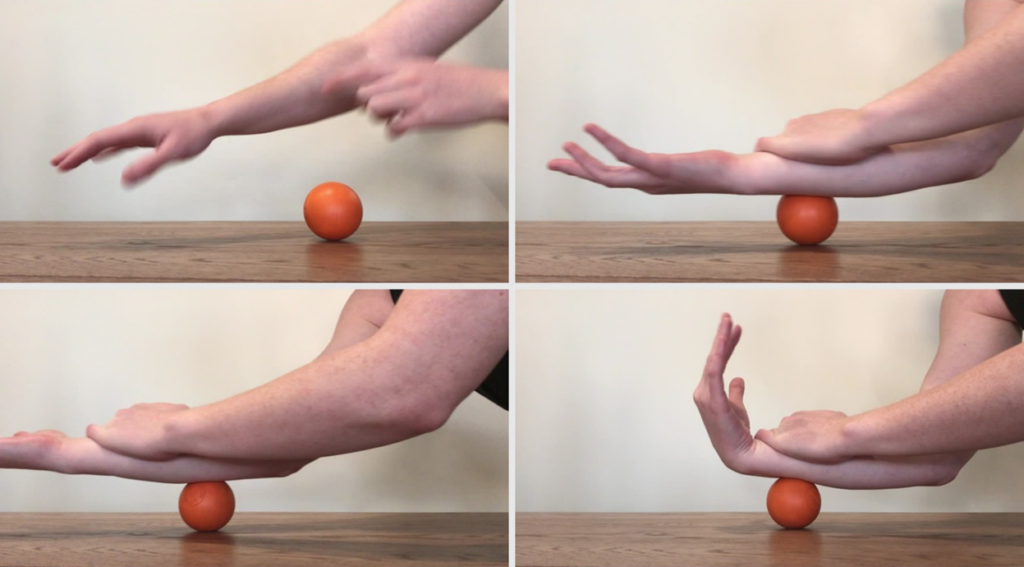
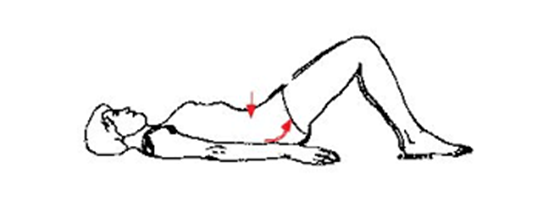
Exercise 3: Leg Pull Preparation
The Leg Pull is a challenging Clinical Pilates exercise for your shoulder blades and core muscles.
- Start on your hands and knees with your hands slightly ahead of your shoulders, then place your knees directly below your hips.
- From here, gently squeeze your shoulder blades together and draw your abdominal muscles up and in, keeping your lower back flat.
- As you exhale, hover your knees off the floor by a few centimetres. Keep the rest of your body still and your neck long.
- As you inhale, hold this position.
- As you exhale, lower your knees back to the mat.
- Repeat this 10 times, ensuring you keep your back flat and your shoulder blades squeezed throughout the exercise.


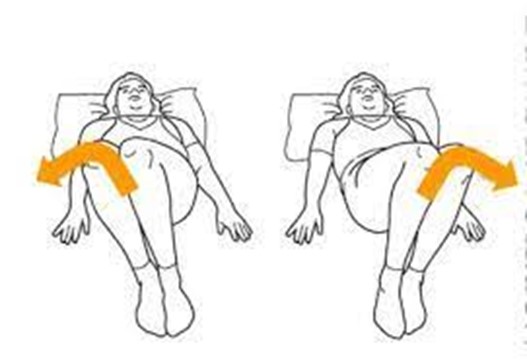
Exercise 4: Arm Openings
For the fourth exercise we have the Arm Openings Clinical Pilates which is beneficial for your upper back and chest muscles.
- Lie on your side with your head supported on a pillow with your knees stacked and bent to 90 degrees. Then rest your arms in front of you.
- As you breathe out, take your top arm and reach towards the ceiling and then out to the side. Open through your chest and let your head move gently with you.
- When you feel a stretch through your chest or back, hold this position and take a deep breath in.
- As you breathe out, return back to the starting position.
- Complete this 6 times
- Repeat on the opposite side.


*Please note: not all exercises are appropriate for all people. If you feel dizzy, have increased pain, or have troubles breathing while completing these exercises, please stop the exercise. Then consult with a medical professional. If you have a history of chronic neck, shoulder or lower back pain, it is recommended to see a physiotherapist first and ensure the most appropriate exercises are prescribed for your condition. ***
I hope you give these Clinical Pilates exercises a try to help with your posture. Doing these exercises once per day or mixing them up throughout your day can be helpful to keep your body moving well and feeling great! If you are interested in learning more about Clinical Pilates, please give us a call at 403-343-8891. Our Clinical Pilates Physiotherapist in Red Deer would be happy to help you feel stronger and move better. You can also click here to book with her.