3 Tips to Prevent Shin Splints For Runners
By Blake Goehring, Physiotherapist
Shin splints can be a serious buzz kill to your summer activity plans. Once shin splints start, they are hard to get rid of without taking your foot off the proverbial gas pedal. Shin splints will be noticeable as pain on the front of your lower legs with any activity such as walking or running. So let’s learn how to prevent shin splints!
The Two Types of Shin Splints
Type #1: Medial Shin Splints
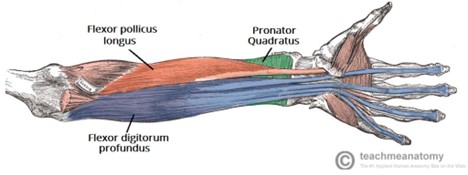
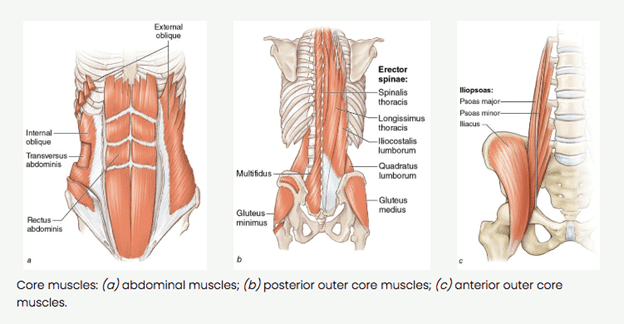
Typically, this pain starts on the inside of your shin bone and is caused by the repeated collapse of the arch of the foot. In this case, tibialis posterior, a muscle in charge of maintaining the arch, is usually what gets overworked and becomes the pain generator. Medial shin splints can occur when there is weak muscular control around your ankle and hyper-mobility in your feet.
Type #2: Lateral Shin Splints
This pain is found on the outside of the main shin bone and is caused by high ground reaction forces, such as heel striking when walking or running. Tibialis anterior, a muscle in charge of lowering the foot after heel contact, is usually what gets overworked in this case. As a result, it is the pain generator with lateral shin splints.
3 Tips to Prevent Shin Splints
Tip #1: Run Quietly!
Most of us distract or motivate ourselves with music while walking or running. In effect, this prevents us from focusing on our mechanics. It stops us from listening to how loud we are on our feet. Unplugging from music can help us be more aware of the force that our feet strike the ground with during a stride. A good place to notice this is on a treadmill. Here, the environment is slightly more controlled. Reduce your noise by the following:
- Removing your shoes for a short period of time while running on a treadmill. If you are running loudly, it will hurt your feet and cause you to absorb force more efficiently.
- Be aware of how much your head is moving up and down while running. Less vertical displacement = less force on the feet and shins.
- Increase your cadence (number of steps you take per minute). Increasing your number of strides can encourage more movement directed forward rather than vertically. The goal is 160-180 steps per minute.
Tip #2: Wear proper footwear.
It is easy to get caught up in the trend of barefoot running or extremely cushioned shoes. The truth is you need to find the shoe that fits you best based on your running style, profile of your feet, and the terrain you run on. If you are a heel striker by nature, a minimalist shoe is likely not appropriate. In a similar light, if you are a forefoot striker, a very cushioned heel through the shoe doesn’t make sense.
When it comes to the profile of your feet, both your arch control and flexibility of your feet matter greatly. If you have dynamic arch collapse (i.e. when you stand on one foot, your arch flattens) or if you have hyper-flexible feet, a shoe that offers more support makes more sense. If you have good muscular control and endurance in your feet and ankles, a minimalist shoe is usually a better fit for you.
There is a lot of context that goes into picking the correct footwear, so ask your physiotherapist next time you are at the clinic for more guidance.
Tip #3: Be progressive.
If you present your body with subtle changes to your training volume, terrain, and intensity, your body will thrive. A common mistake to avoid is changing one of those parameters drastically; e.g. start by running 10KM in the first week of training. In these cases, the body is unable to adapt to these changes which leads to an injury. In general, small, incremental changes in your intensity are good ways to start increasing your running without hurting yourself. E.g., increasing speed by 10 seconds per kilometre.
Avoiding shin splints is as easy as starting with a plan. If this is a common issue you suffer from or you want more detailed information, make an appointment with a physiotherapist at Stride to ensure you have a fun filled summer without injuries! Click here to book now.