4 Tips for Preventing Back Injuries This Winter
By: Devan Mercereau, Physiotherapist
As beautiful as they are, winters in our province are cold and snowy! Which leads to back injuries for a lot of reasons. When a storm hits, so does our responsibility to go outside and clear our sidewalks and driveways from snow. Most of us have been there; bundling up from head to toe, facing the grueling cold to clear our driveway, only to have to go out and repeat the whole process an hour later. As tedious as it is, rushing this annoying winter chore can have consequences. In addition to winter sports and icy conditions, shoveling snow can be the culprit behind many injuries this time of year.
Here are my top 4 tips for shovelling snow so you can stay safe, prevent back injuries, and enjoy all the great winter activities Alberta has to offer!
Tip #1: Body Position
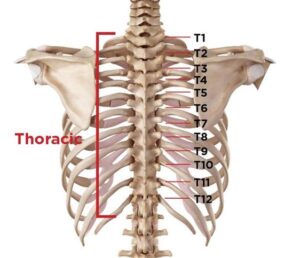
Body positioning and proper mechanics are some of the most important aspects of any activity. I understand this as I have experienced issues with my own lower back from playing sports and growing up with scoliosis (curvature in the spine).
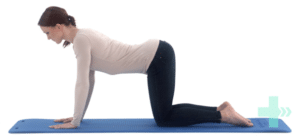
When shoveling snow, consider this checklist for proper body positioning and mechanics:
– Hinge at the hips
– Have a slight bend in the knees
– Place your feet about hip width apart, creating a larger base of support
– Keep the shovel close to your body to avoid reaching
– Avoid twisting and throwing snow
Tip #2: Mindfulness When Shoveling
Being aware of proper body positioning when shoveling can help prevent injuries. It’s easy to forget about maintaining good posture and body positioning when it is freezing cold and the snow is blowing all around. Shoveling smart and pacing yourself can help to avoid extra strains on the body. This correlates with tip #1!
It is also wise to think about the type of snow you are shoveling. Sounds strange, right? Even if the fluffy stuff seems effortless to move, it’s also easier to forget about proper body positioning, causing extra strain from repetitive twisting or movements. Similarly, wet snow can be heavy, creating an opportunity for overexertion and fatigue. Evaluate your conditions every time you go outside!
Finally, be aware of the amount of shoveling required. If you have a large driveway, taking small breaks throughout the process decreases the strain on the lower back from continuous repetitive movements.
Tip #3: Pushing Smaller Amounts of Snow
I know what you are thinking, smaller loads = more time shoveling! But the extra time investment could pay off.
Depending on the snowfall, the weight and density of the snow can change quickly. So, pushing smaller and lighter piles can decrease the load on your spine. Although it may take more time to remove, the decreased risk of injury may be worth it.
Tip #4: The Type of Shovel
A durable, lightweight shovel can decrease the load on the body when pushing snow around. Using a shovel with a curved handle also improves body positioning because it allows us to keep our spine in a more neutral position, rather than hunching forward over a straight handle. If your shovel is too big and cumbersome, try swapping it for a smaller model and embrace tip #3!
If you are experiencing any lower back pain or want to improve strength and conditioning for functional activities, feel free to reach out to our clinic or book an appointment online by clicking here.